A nurse is preparing a sterile field, a critical procedure in healthcare settings to prevent infections during invasive procedures. This comprehensive guide delves into the essential steps, materials, and techniques involved in creating and maintaining a sterile field, ensuring patient safety and optimal outcomes.
Maintaining sterility is paramount in healthcare to prevent infections and ensure patient well-being. This guide provides a step-by-step approach to preparing a sterile field, covering essential materials, infection control measures, sterilization techniques, and quality control practices.
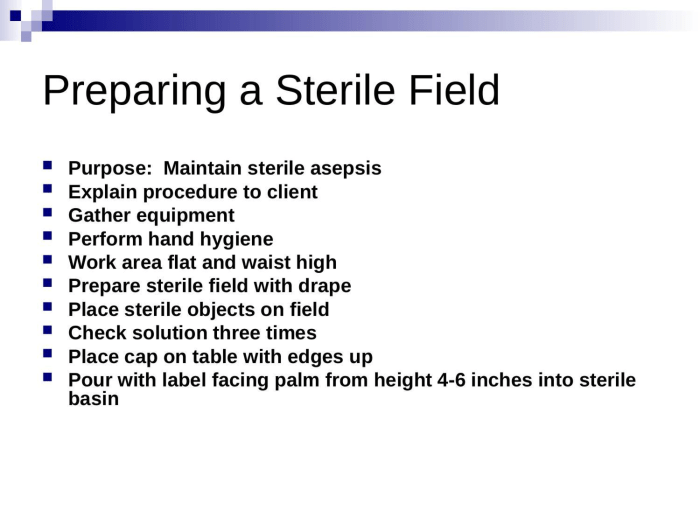
Preparation Procedures
Maintaining sterility during a sterile field procedure is paramount to prevent contamination and ensure patient safety. A sterile field is an area free of microorganisms, created to perform aseptic techniques, such as injections, wound care, and surgical procedures.
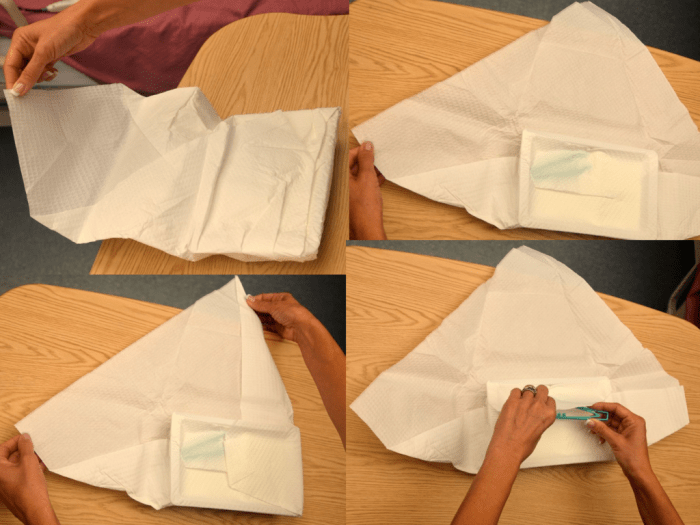
Setting up a sterile field requires meticulous attention to detail. Begin by gathering necessary sterile materials, including a sterile drape, gloves, gown, mask, and instruments. Ensure the work surface is clean and free of debris. Open the sterile drape aseptically and place it on the work surface, folding the edges to create a barrier.
Handling Sterile Instruments and Materials
Once the sterile field is established, handle sterile instruments and materials with utmost care. Use sterile forceps or gloves to transfer items to and from the field. Avoid touching the sterile surfaces of instruments or the drape. If contamination occurs, discard the item immediately and set up a new sterile field.
Remember, maintaining a sterile field is an ongoing process that requires constant vigilance and adherence to best practices. By following these guidelines, healthcare professionals can ensure the safety and integrity of sterile procedures.
Materials Required
Creating a sterile field necessitates an array of materials, each playing a crucial role in maintaining sterility throughout the procedure. These materials possess specific characteristics and require proper handling to ensure their effectiveness.
Sterile Drapes
Sterile drapes are large, sterile fabrics used to cover surfaces, equipment, and the patient to create a sterile field. They are made of non-woven materials such as polyester or polypropylene, which are impervious to fluids and bacteria.
Sterile Gloves
Sterile gloves are worn by healthcare professionals to prevent the transfer of microorganisms between their hands and the sterile field. They are made of latex or nitrile and come in various sizes to ensure a snug fit.
Sterile Gowns
Sterile gowns are worn by healthcare professionals to protect their clothing and skin from contamination. They are made of fluid-resistant materials such as polyethylene or polypropylene and have long sleeves, a closed back, and a tie or Velcro closure.
Sterile Masks, A nurse is preparing a sterile field
Sterile masks are worn by healthcare professionals to prevent the spread of microorganisms through respiratory droplets. They are made of non-woven materials such as polypropylene or cellulose and have a filtration efficiency of at least 95%.
Sterile Table
A sterile table is a small, portable table covered with a sterile drape. It is used to hold sterile instruments and materials during a procedure.
Sterile Basin
A sterile basin is a shallow, round container used to hold sterile solutions or instruments. It is made of stainless steel or plastic and has a lid to prevent contamination.
Sterile Syringes and Needles
Sterile syringes and needles are used to administer medications or fluids. They are made of glass or plastic and are individually packaged to maintain sterility.
Sterile Alcohol Sponges
Sterile alcohol sponges are used to clean the skin before an injection or procedure. They are made of cotton or gauze soaked in 70% isopropyl alcohol.
Sterile Cotton Balls
Sterile cotton balls are used to absorb fluids or clean wounds. They are made of 100% cotton and are individually packaged to maintain sterility.
Sterile Adhesive Tape
Sterile adhesive tape is used to secure dressings or other items to the skin. It is made of hypoallergenic materials such as paper or plastic and has a strong adhesive backing.
Proper Storage and Handling
To ensure the sterility of materials, proper storage and handling techniques are essential. Sterile materials should be stored in a clean, dry environment away from direct sunlight and heat. They should be kept in their original packaging until ready for use and should not be touched with bare hands.
Infection Control Measures: A Nurse Is Preparing A Sterile Field
Infection control is of paramount importance during surgical procedures to prevent the risk of surgical site infections (SSIs). SSIs can prolong hospital stays, increase healthcare costs, and potentially lead to severe complications. Therefore, adhering to strict infection control measures is crucial to ensure patient safety and optimal outcomes.
Preventing Contamination of the Sterile Field
The sterile field is an area created around the surgical site to minimize the risk of contamination. Maintaining the integrity of the sterile field is essential to prevent the introduction of microorganisms into the surgical wound. This can be achieved by:
- Restricting access to the sterile field to authorized personnel only.
- Using sterile drapes, gowns, and gloves to create a physical barrier between the surgical team and the patient.
- Avoiding unnecessary movement within the sterile field.
- Handling sterile instruments and materials with care to prevent accidental contact with non-sterile surfaces.
Proper Use of Personal Protective Equipment (PPE)
PPE is worn by the surgical team to protect themselves and the patient from potential exposure to infectious agents. Proper use of PPE includes:
- Wearing a surgical gown that covers the body and prevents the transfer of microorganisms from the surgeon’s clothing to the patient.
- Wearing sterile gloves that create a barrier between the surgeon’s hands and the surgical site.
- Wearing a surgical mask that prevents the spread of respiratory droplets.
- Wearing eye protection, such as goggles or a face shield, to prevent splashes or aerosols from entering the eyes.
Sterilization Techniques

Sterilization is the complete elimination or destruction of all forms of microbial life, including spores. It is a critical step in infection control to prevent the transmission of microorganisms from contaminated instruments and materials to patients.There are various methods used to sterilize instruments and materials, each with its own advantages and disadvantages.
The choice of sterilization method depends on the type of item being sterilized, the level of sterility required, and the availability of resources.
Physical Methods
- Heat Sterilization:Heat sterilization involves exposing items to high temperatures to kill microorganisms. It can be achieved through dry heat (e.g., hot air oven) or moist heat (e.g., autoclave). Dry heat is suitable for heat-stable materials, while moist heat is more effective for penetrating porous materials.
- Radiation Sterilization:Radiation sterilization uses high-energy radiation, such as gamma radiation, to kill microorganisms. It is a reliable and effective method, but it requires specialized equipment and can damage some materials.
- Filtration:Filtration is used to remove microorganisms from liquids or gases by passing them through a filter with pores small enough to trap microorganisms.
It is a common method for sterilizing fluids, such as intravenous solutions and vaccines.
Chemical Methods
- Chemical Sterilization:Chemical sterilization involves using chemical agents, such as ethylene oxide or hydrogen peroxide, to kill microorganisms. It is suitable for heat-sensitive materials that cannot withstand high temperatures. However, chemical sterilization can leave residues on the items, which may need to be removed before use.
- Disinfection:Disinfection is a less stringent form of sterilization that kills most, but not all, microorganisms. It is often used for non-critical items, such as environmental surfaces and medical devices that come into contact with intact skin.
Proper Sterilization Procedures
To ensure effective sterilization, it is crucial to follow proper procedures. This includes:
- Cleaning and preparing the items to be sterilized.
- Selecting the appropriate sterilization method based on the item’s characteristics.
- Using the correct exposure time and temperature for the chosen method.
- Verifying the sterility of the items using appropriate methods, such as biological indicators.
By adhering to these procedures, healthcare professionals can ensure the safety of patients and prevent the transmission of infections through contaminated instruments and materials.
Quality Control

Maintaining sterility is paramount in healthcare settings, as it directly impacts patient safety and the effectiveness of medical interventions. Quality control plays a pivotal role in ensuring the integrity of sterile fields and preventing contamination.
To monitor the effectiveness of sterilization techniques, various methods are employed:
Chemical Indicators
- Chemical indicators change color or form in response to specific sterilization conditions, such as temperature, humidity, or chemical exposure. These indicators are placed within the sterile field and monitored after the sterilization process to verify its efficacy.
Biological Indicators
- Biological indicators contain viable microorganisms that are highly resistant to sterilization. Their survival after the sterilization process indicates a failure in the sterilization technique.
Physical Indicators
- Physical indicators, such as pressure gauges and thermometers, monitor the physical parameters of the sterilization process, ensuring that they meet the required specifications.
Regular monitoring and maintenance of sterilization equipment are crucial to prevent contamination. Common problems encountered during the preparation of a sterile field include:
Troubleshooting
- Leaking or damaged packaging:Replace the packaging immediately and re-sterilize the contents.
- Failure of chemical or biological indicators:Investigate the cause of the failure and repeat the sterilization process.
- Physical parameter deviations:Recalibrate the equipment and repeat the sterilization process.
- Improper storage:Ensure sterile items are stored in a clean, dry, and temperature-controlled environment.
Adherence to quality control measures and prompt troubleshooting are essential to maintain the sterility of the operating environment and ensure the safety and well-being of patients.
Commonly Asked Questions
What is the purpose of a sterile field?
A sterile field is an area that has been made free of microorganisms to prevent infection during invasive procedures.
What are the essential materials needed for preparing a sterile field?
Essential materials include sterile gloves, gowns, masks, drapes, instruments, and solutions.
How do you properly sterilize instruments and materials?
Sterilization methods include autoclaving, chemical sterilization, and radiation.
What are the key infection control measures during sterile field preparation?
Key measures include hand hygiene, proper use of personal protective equipment, and maintaining aseptic technique.